Endometrial receptivity and fertility
- Dr. Jaime DeGuzman, DTCM, L.Ac

- Mar 27
- 6 min read
Many factors are involved in a successful pregnancy, but without a doubt the quality of the uterine lining plays a very important role. During the short window of implantation the uterine lining has to be in optimal conditions to receive the embryo.

Background
As a woman goes through her menstrual cycle, the endometrium (uterine lining) goes through several phases. The proliferative phase, the first phase of the menstrual cycle, is mainly driven by estrogen. During this phase new blood vessels develop and endometrial cells multiply and increase in size to supply the growing and thickening endometrium. This phase typically lasts from days 1 to 14 of the menstrual cycle.
The secretory phase, which occurs after ovulation and before menstruation, is a crucial part of the menstrual cycle and a key factor in female fertility. Driven by progesterone, the main purpose of this phase is to create a suitable environment for implantation and provide nourishment to the growing embryo if fertilization occurs. During this phase the endometrium thickens and it appears more spongy, the spiral arteries in the endometrium widen to increase blood flow, and in preparation for potential pregnancy, the cells of the endometrium begin to show signs of transformation ("decidualization"). The secretory phase typically lasts about 14 days, from ovulation until menstruation begins. It is important to note that if the endometrium does not develop properly during this phase, implantation may be impaired, leading to infertility or miscarriage.
Introduction
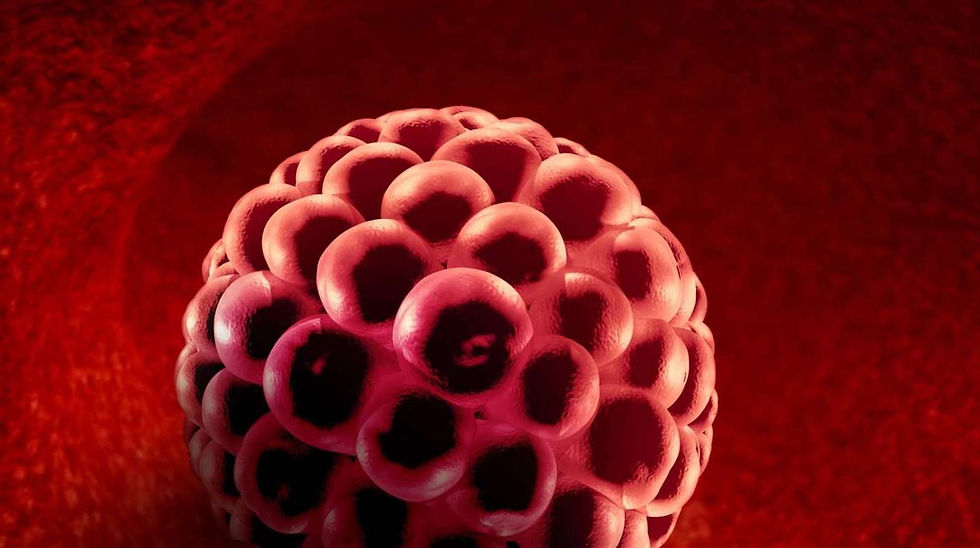
Endometrial receptivity has been defined as the period of endometrial maturation during which the outer edge of the blastocysts (early-stage embryo) can attach to the endometrial epithelial cells and subsequently invade the blood vessels that supply the endometrium. Aside from being a very delicate process where the blastocyst and the endometrium are in perfect synchronization, there is a very short window when this can take place. The limited period of optimal endometrial receptivity in which the endometrium is ready to receive an embryo and the embryo is ready to be implanted, is commonly referred to as the "window of implantation". On a normal 28-day menstrual cycle this window is generally detected between cycle days 20 and 24. Outside this window, the endometrium is completely resistant to implantation.
Decidualization
Decidualization is the process of intense tissue remodeling that transforms the cycling endometrium into a dynamic tissue, the decidua, in preparation for pregnancy. During this process the uterine lining goes through many changes, including the transformation of endometrial stromal cells into decidual stromal cells, and the transformation of uterine glands into secretory glands. Decidualization is a key part of early pregnancy. Many experts believe that the foundation for a healthy pregnancy is laid prior to the establishment of the pregnancy at the time of endometrial decidualization. An article published in 2020 by the International Journal of Molecular Medicine where several studies are mentioned, declares that there is increasing evidence to suggest that the quality of the soil (endometrium)—a process known as decidualization—may contribute more to reproductive disorders than the quality of the seed (embryo).
Progesterone and decidualization
Progesterone is an essential regulator of decidualization and a prerequisite for successful blastocyst implantation. Endometrial stromal cells have progesterone receptors which allow the transformation into decidual stromal cells at the encounter of progesterone. With insufficient progesterone, the endometrial stromal cells will not transform into decidual stromal cells - decidualization does not take place. According to a study published in 2018 by Reproductive Medicine and Biology, progesterone signaling (via Progesterone Receptors) is essential for decidualization and is a prerequisite for a successful implantation. The study summarizes its findings by saying that:
“ These findings indicate that progesterone is the master regulator of pregnancy in both humans and mice”.
Prolactin and decidualization
Prolactin is well known as the hormone that helps women produce milk – lactate. It is also well understood that high levels of prolactin – like when a new mother is lactating, can prevent a woman from getting pregnant. A less known role of prolactin is during the process of decidualization. After ovulation the levels of progesterone rise and decidualization takes place. At this time decidualized endometrial stromal cells begin to secrete prolactin. As mentioned by a study published in 2023 by Frontiers in Immunology, in addition to the pituitary gland, especially decidualized endometrial stromal cells also produce prolactin. Prolactin plays a crucial role in decidualization by regulating genes involved in the process, maintaining progesterone production, and influencing endometrial vascularization to support implantation.
While it is clear that the release of prolactin by the decidualized cells is a sign of a decidualized endometrium, the exact timing of the onset of prolactin in the luteal phase has been controversial. A study by Gynecological Endocrinology published in 2020 shows that prolactin was detected in the late-luteal phase, but some studies indicated its onset from as early as day 24.
“ Prolactin plays a crucial role in decidualization by regulating genes involved in the process, maintaining progesterone production, and influencing endometrial vascularization to support implantation”.
Timing is everything
The blastocysts and the endometrium have to be ready at the same time – embryo-endometrial synchrony, for implantation to take place. If the blastocyst is ready, but the endometrium is not, or vice-versa, implantation will not take place. The study by Gynecological Endocrinology, mentions that:
“ Premature advancement of endometrial decidualization may lead to embryo–endometrial asynchrony, resulting in dysfunctional embryo–endometrial interaction and consequently implantation failure”.
Since prolactin is one of the hormones secreted by decidualized endometrial stromal cells, it can be used as a marker to detect if decidualization has taken place. While the levels of prolactin fluctuate during the menstrual cycle, there is some evidence showing that a luteal phase defective endometrium produces less prolactin than normal control endometrium. According to an old study published in 1979 by Fertility and Sterility, the amount of prolactin during the early luteal phase is 15.6 ± 2.9 ng/ml and 13.9 ± 2.8 ng/ml during the late luteal phase.
Endometrium thickness
The thickness of the lining is crucial for a successful implantation. While many reproductive endocrinologists say that the lining needs to be at least 8mm before implantation, a study done in 2009 reported that there were significantly more pregnancies in the 7 – 14 mm endometrial thickness group compared to the <7 mm and >14mm groups.
Endometrium appearance
A trilaminar endometrial lining, often visualized on ultrasound as a three-layered appearance, is generally considered a positive sign and is correlated with a higher pregnancy rate. A study aimed to see if there is correlation between a trilaminar endometrial pattern and higher clinical pregnancy rates was conducted by Fertility and Sterility. The study was published in 2017 and concluded that:
“ While endometrial thickness is an important sonographic marker of endometrial receptivity, the present data show that a trilaminar endometrial appearance is also a significant, independent predictor of implantation with a 3-fold increase in CPR (Clinical Pregnancy Rate) in FET cycles”.
Acupuncture and the lining
There’s evidence indicating that acupuncture may improve endometrial receptivity by enhancing blood flow to the uterus, regulating neuroendocrine factors, and potentially modulating the immune response. A study aimed at understanding the effect of acupuncture on endometrium and pregnancy outcomes in patients with polycystic ovary syndrome undergoing IVF was published in 2022 by The Chinese Journal of Integrative Medicine. The study randomly assigned 83 patients into two groups; the Acupuncture group received 3 courses of acupuncture from the time of ovulation induction until the day of the embryo transfer. The control group did not receive acupuncture. The study concluded by saying that:
“ Acupuncture can improve the proportion of type A endometrium, regulate the levels of serum E2 (estradiol) and P (progesterone) on the day of hCG injection, and improve the pregnancy rate in patients with PCOS infertility undergoing IVF-ET”.
In addition, research suggests that moxibustion, particularly when combined with acupuncture, can improve endometrial receptivity and increase the clinical pregnancy rate in patients with infertility or recurrent implantation failure. For example, one study found that warming-needle moxibustion can increase endometrial thickness, thus improving endometrial receptivity, enhancing embryo implantation rate, and improving pregnancy outcome.
Conclusion
There’s plenty of research suggesting that the quality of the lining is more important than the quality of the embryo – the soil is more important than the seed. If endometrial decidualization does not occur, a process driven by progesterone, implantation will not take place. Acupuncture, as well as moxibustion, has been shown to have a positive effect on improving the quality of the lining.





Comments