ERA - Endometrium Receptivity Analysis
- Dr. Jaime DeGuzman, DTCM, L.Ac

- Oct 26
- 4 min read
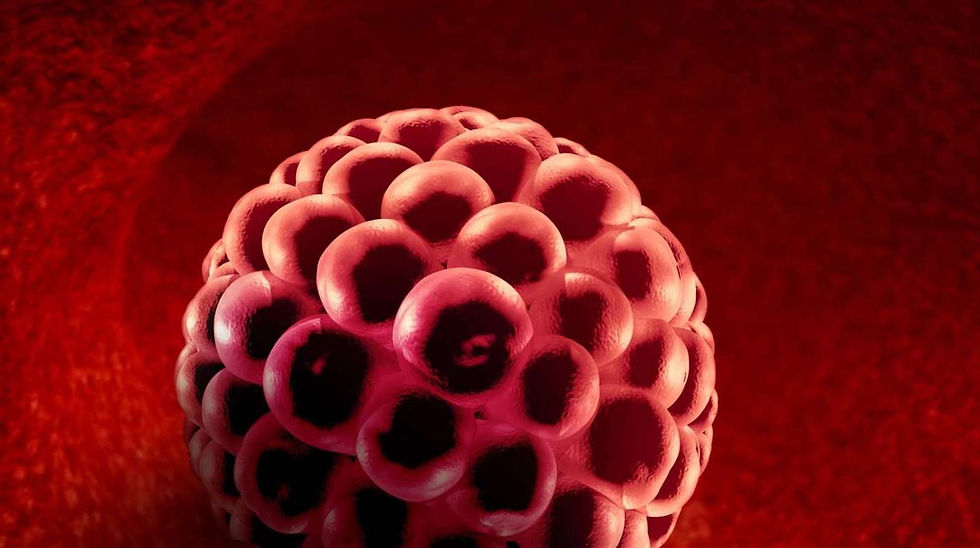
To identify the optimal window of implantation for embryo transfer and improve the chances of a successful pregnancy, a diagnostic procedure known as Endometrial Receptivity Analysis (ERA) is performed in women undergoing an IVF cycle.
Background
According to a meta-analysis review published by Human Reproductive Update in 2019, suboptimal endometrial receptivity is estimated to account for up to two-thirds of implantation failures. In an effort to better understand the optimal time to transfer an embryo and reduce the rate of implantation failures, some reproductive endocrinologists believe that by taking and analyzing a small sample of the uterine lining they can predict the best time to transfer an embryo. While ERA has been used for many years by multiple fertility clinics, data from a study released in 2021 shows that the findings do not support routine use of receptivity testing to guide the timing of embryo transfer during an IVF cycle.
Introduction
A review by the journal of Human Reproduction released in the year 2000, explains that in a typical 28-day menstrual cycle, the window of implantation is generally considered to be between cycle days 20 and 24. The review continues by saying that implantation outside this window is markedly reduced. During an IVF cycle, where the menstrual cycle is manipulated by different medications, the window of implantation is estimated by the timing and duration of progesterone exposure following ovulation or trigger. While progesterone is essential for transforming the endometrium from a proliferative to a receptive state, enabling embryo implantation, studies also show that adequate estrogen priming initiates secretory changes, decidualization, and the expression of key genes and proteins required for receptivity.
Despite careful control of estrogen and progesterone levels at precise times, many IVF embryo transfers still fail—even when using genetically tested, high-quality embryos. This ongoing challenge inspired the idea of taking a biopsy of the uterine lining before embryo transfer to determine whether the endometrium is truly receptive and ready to support implantation.
What is ERA
Endometrial receptivity analysis (ERA) is a diagnostic test that evaluates the gene expression of an endometrial biopsy to determine the best time to transfer an embryo. By assessing the expression of hundreds of genes associated with endometrial receptivity, ERA classifies the endometrium as pre-receptive, receptive, or post-receptive, allowing for a personalized embryo transfer based on the individual's window of implantation rather than standardized timing.
A Mock Cycle
The ERA procedure includes a “mock” cycle, which is a practice cycle designed to replicate the conditions of a real embryo transfer, but without actually transferring an embryo. During this cycle, the uterine lining (endometrium) is prepared using the same hormone treatments as in a real transfer. The main difference is that, instead of transferring an embryo, a small biopsy of the endometrium is taken at the expected window of implantation to check how receptive it is. The test results show whether the endometrium is receptive, pre-receptive, or post-receptive at that time. If the results indicate that the window of implantation is shifted, the timing of progesterone or the embryo transfer can be adjusted in future cycles to improve success.
How Successful is ERA
While some studies have reported modest improvements in pregnancy outcomes, these findings often apply to specific subgroups—such as patients with previous failed embryo transfers or recurrent implantation failure (RIF). For example, one study involving 281 patients with RIF found that ERA-guided personalized embryo transfer (pET) significantly improved pregnancy and implantation rates compared with conventional frozen embryo transfer (FET). On the other hand, multiple high-quality studies have found no significant difference in live birth rates, clinical pregnancy rates, or implantation rates when ERA was used prior to embryo transfer compared to standard protocols. For example, a large randomized controlled trial found live birth rates of 58.5% with ERA-guided transfer versus 61.9% with standard timing (P = .38), with no significant differences in secondary outcomes. Similarly, a meta-analysis of over 14,000 patients concluded that ERA does not improve live birth, clinical pregnancy, or implantation rates.
Acupuncture and Endometrium Receptivity
There is some evidence that acupuncture might help improve the uterine lining by increasing blood flow to the uterus, balancing hormone levels, and possibly affecting the immune system. In 2022, The Chinese Journal of Integrative Medicine published a study on acupuncture’s effects on the uterine lining and pregnancy rates in patients with polycystic ovary syndrome (PCOS) undergoing IVF. The study included 83 patients who were randomly divided into two groups. One group received three courses of acupuncture from ovulation induction until the day of embryo transfer, while the other group did not receive any acupuncture. The study concluded by saying that:
“ Acupuncture can improve the proportion of type A endometrium, regulate the levels of serum E2 (estradiol) and P (progesterone) on the day of hCG injection, and improve the pregnancy rate in patients with PCOS infertility undergoing IVF-ET”
In addition, research suggests that moxibustion, particularly when combined with acupuncture, can improve endometrial receptivity and increase the clinical pregnancy rate in patients with infertility or recurrent implantation failure. For example, one study found that warming-needle moxibustion can increase endometrial thickness, thus improving endometrial receptivity, enhancing embryo implantation rate, and improving pregnancy outcome.
Conclusion
Endometrial receptivity is crucial for successful embryo implantation, whether conception is natural or assisted. While modern technologies like the Endometrial Receptivity Analysis (ERA) aim to pinpoint the best timing for embryo transfer, their results remain mixed and inconclusive. In contrast, traditional Chinese medicine offers a holistic approach, focusing on restoring balance and harmony within the body to naturally create a receptive uterine environment. By addressing the body’s overall energy and health, ancient practices may provide valuable support in enhancing fertility and improving implantation success.






Comments