Fertility Tools and Stress
- Dr. Jaime DeGuzman, DTCM, L.Ac

- Sep 29
- 3 min read
Ovulation Predictor Kits (OPK) are becoming very popular and very sophisticated. Women who are trying to conceive are depending on OPKs to let them know when they will ovulate so that they can start to TTC – trying to conceive.

Background
Since their introduction in the late 1980s, at-home Ovulation Predictor Kits (OPKs) have become increasingly popular among women trying to conceive (TTC). These kits enable women to predict ovulation from the comfort of their own homes by detecting the surge of Luteinizing Hormone (LH) in urine. A rise in LH typically indicates that ovulation will occur within 24 to 36 hours, making OPKs a convenient and accessible tool for identifying a woman’s fertile window.
Introduction
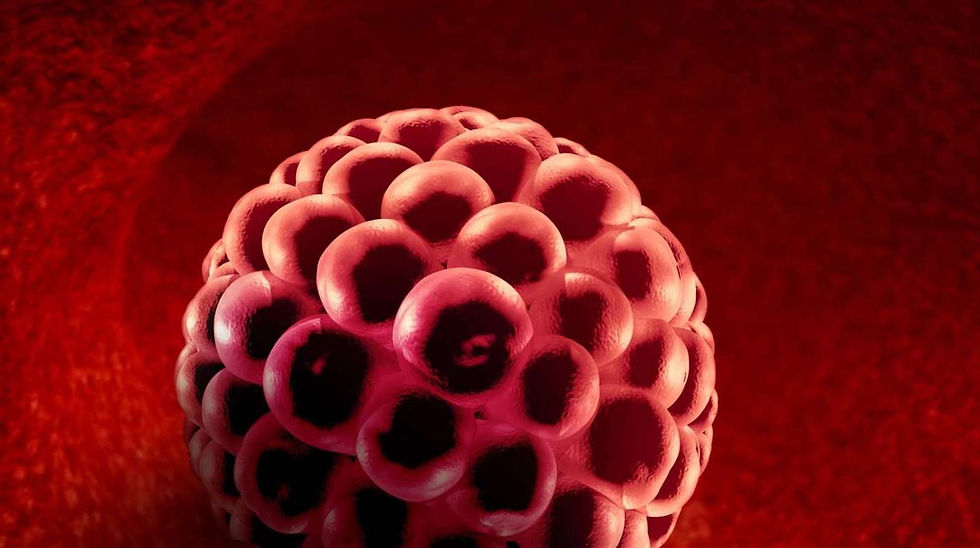
Once ovulation occurs, the released egg remains viable for fertilization for approximately 12 to 18 hours. With such a narrow window, OPK manufacturers market their products as essential tools for couples hoping to conceive, especially those who have been trying unsuccessfully for extended periods. Alongside OPKs, a wide range of fertility monitoring tools are now available, including those that measure Follicle Stimulating Hormone (FSH), Estradiol, Basal Body Temperature (BBT), and pregnancy status. These tools have become integrated into many users' daily routines.
Common Misuse of OPKs
A common mistake made by couples TTC is timing intercourse to coincide with ovulation based solely on OPK results. While conception can occur on the day of ovulation, studies show that the chances of pregnancy are significantly higher when intercourse takes place one to two days prior to ovulation. Waiting for a positive OPK result to initiate intercourse may result in missed opportunities for conception.
Fertility Tools and Psychological Impact
Modern fertility technologies, including smartphone apps, wearable devices, and testing kits, provide detailed information about various biomarkers. While this data can empower users, it can also lead to information overload, anxiety, and stress—particularly when results are inconsistent or difficult to interpret. Research has shown that many fertility apps fail to accurately identify fertile windows, with only 4 out of 53 platforms performing as intended. Moreover, these tools can unintentionally reinforce societal expectations surrounding reproductive responsibility and put strain on relationships when conception does not occur as expected.
A More Natural Approach
Understanding and observing natural fertility indicators—such as cervical mucus (CM) changes and shifts in libido—can provide more accurate and holistic insights into ovulation. For instance, cervical mucus that is clear, stretchy, and slippery (often compared to egg whites) typically indicates that a woman is in her fertile window. Similarly, an increase in sexual desire is a biological signal that ovulation is approaching.
A woman who is attuned to her body’s natural signs of fertility can begin attempting to conceive up to five days before ovulation. This strategy takes advantage of the fact that healthy sperm can live in the female reproductive tract for up to five days. For women with irregular ovulation patterns, such as those with Polycystic Ovary Syndrome (PCOS), it is advisable to have intercourse at least twice per week to maximize the likelihood of conception.
Leave Biomarker Interpretation to Experts
While biomarkers are essential for understanding reproductive health, daily or excessive self-monitoring is not necessary and can lead to confusion. Urine-based hormone tests offer limited accuracy compared to serum (blood) tests. Fertility specialists should conduct comprehensive hormone panels at specific points in the menstrual cycle, interpreting results within the context of the patient’s overall health and providing personalized recommendations on improving fertility through diet, lifestyle changes, supplements, and other interventions.
Conclusion
Although technological fertility aids can offer valuable insights, they may also contribute to increased stress—an established factor that negatively affects fertility. Adopting a more natural approach, including observation of physical signs and stress-reducing practices such as acupuncture, may lead to more balanced and effective fertility outcomes. A combination of expert guidance and personal awareness can empower couples to navigate their fertility journey with confidence and clarity.





Comments